Episode 3
The One Where the Cells Break All the Rules
Ladies and gentlemen, fellow science geeks, and anyone who’s ever wondered why cancer cells act like they’re in a Fast & Furious movie—welcome to episode 3 of 'The Anatomy of a Rebellion'.
Today’s topic of discussion isn’t just about cells misbehaving. Oh no. It’s about 10 bold moves—10 rule-breaking stunts that turn an ordinary cell into a full-blown rebel without a pause button. We’re diving into the Hallmarks of Cancer, a greatest-hits playlist of the worst ways a cell can go rogue.
 |
| Yep , that's cancer(more or less) |
From faking death to ghosting the immune system, from living forever to building blood vessel empires like real estate tycoons, these hallmarks are not your average biology textbook material. But don’t worry—I brought jokes, some mutant p53 tea, and yes, even a suspiciously aggressive cell named RAS who might need therapy.
So buckle up, grab a metaphorical microscope, and get ready to dive in.
Because in the world of cancer biology, the cells aren’t just dividing… they’re planning a heist.
1: “Death? I Don’t Know Her.” — The Curious Case of Cellular Immortality
Okay, so picture this: You’re in your bio class, half-asleep, and the teacher says, “All cells die eventually.” And you go, “Cool, like me after every chemistry exam.” But then — plot twist — some cells don’t.
Some cells don’t die.
Some cells forget how.
And just like that, we’ve entered our first hallmark of cancer: Replicative Immortality.
Meet the Grim Reaper of Cells — Telomeres
Let’s talk telomeres — those weird little shoelace caps at the ends of your chromosomes. Every time your cells divide, telomeres get a little shorter, like the emotional stability of a medical student during finals. Eventually, they’re too short to protect the DNA. That’s when a cell goes, “Welp, time to die,” and gracefully bows out.
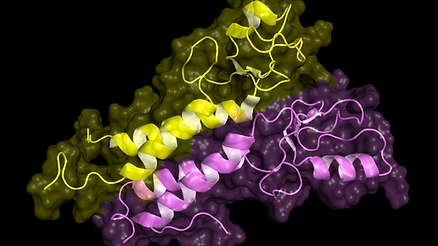
A diagrammatic representation of a chromosomeExcept cancer cells are like that one annoying guest who refuses to leave the party. Ever. Why? Because of a sneaky enzyme called telomerase.
Telomerase — The Forbidden Fountain of Youth
In normal cells, telomerase is either off or very quiet but in most cancer cells, it’s cranked up to 11. Think of it as magical duct tape that keeps the telomeres long and strong.
Scientific sources tell us that about 85–90% of human tumors show upregulated telomerase activity.
So now, our cancer cell has a get-out-of-death-free card. It can keep dividing and dividing — no retirement, no pension plan, just full-time chaos.
But Wait — There’s a Backup Plan!
Not all cancers rely on telomerase. Some use a secret side door called ALT — Alternative Lengthening of Telomeres. It’s rarer, but still powerful, like Voldemort’s backup horcruxes.
ALT works by copying telomeric sequences from one chromosome to another. It’s like cheating on a bio exam by copying someone else’s answers.
Either way, cancer cells win. Immortality unlocked. Mortals: 0, Mutants: 1.
Immortality Sounds Cool… Until It doesn’t
You might be thinking, “Hey, immortality? That’s not so bad!” Sure, if you’re a vampire. But in biology, immortality is the enemy of balance.
Immortal cells mean infinite divisions, which means infinite chances for mutations, which means the rise of cellular Voldemorts with zero chill.
In fact, replicative immortality is like giving a toddler unlimited sugar and zero supervision. Things get ugly real quick.
If that was too confusing , here's a short summary :
Telomeres are like Michael
Scott’s common sense — slowly deteriorating over time.Telomerase? Dwight Schrute with a fire extinguisher, frantically putting out aging signals so the cell can keep “working.”
Finally, just like Creed somehow showing up in every episode unbothered and unchanged, cancer cells just don’t know when to quit.
Telomerase putting out aging signals (not really but kind of )
Replicative immortality is often not the first mutation, but it’s the one that seals the deal. It ensures the cell will keep dividing — and keep spreading its twisted legacy.
And now that we’ve unmasked this villain, guess what?
There are nine more.
2: "Genomic Instability and Mutation: The DNA Rollercoaster"
Imagine your DNA as a meticulously written instruction manual. Now, picture someone spilling coffee on it, tearing out pages, and scribbling notes in the margins. Welcome to the chaotic world of Genomic Instability and Mutation, our second hallmark of cancer.
The Guardians of the Genome
In healthy cells, there's a robust system in place to maintain DNA integrity. Think of it as a team of vigilant editors:
Proofreaders: Enzymes that check for errors during DNA replication.
Repair Crew: Mechanisms like mismatch repair (MMR) that fix any mistakes.
Security Guards: Tumor suppressor genes like p53 that halt the process if something goes awry.
But in cancer cells, these guardians are often compromised. Mutations in genes responsible for DNA repair, such as MLH1 or BRCA1, can lead to a cascade of errors, allowing mutations to accumulate unchecked.
The Mutation Accumulation
With the repair systems down, the cell's genome becomes a playground for mutations. These changes can:
Activate oncogenes, pushing the cell to divide uncontrollably.
Inactivate tumor suppressor genes, removing the brakes on cell division.
Create chromosomal abnormalities, like translocations or duplications.
This genomic chaos provides cancer cells with a survival advantage, enabling them to adapt to hostile environments, resist therapies, and metastasize to new locations.
If Cancer Biology Was a TV Show…
Friends Edition:
DNA Repair Mechanisms: Think of Monica's obsessive cleanliness. She ensures everything is in order, much like DNA repair systems maintain genomic integrity.
Genomic Instability: Now, imagine Joey trying to clean the apartment. He means well but ends up creating more mess—akin to faulty repair mechanisms introducing more mutations.
Cancer Cells: They're like Ross's multiple divorces. Each one adds complexity and drama, reflecting how accumulating mutations complicate the cell's behavior.
Therapeutic Implications
Understanding genomic instability has paved the way for targeted therapies:
PARP Inhibitors: Effective against tumors with BRCA mutations, exploiting the cancer cell's compromised DNA repair pathways.
Checkpoint Inhibitors: Targeting cells with high mutation burdens, making them more recognizable to the immune system.
However, the adaptability conferred by genomic instability also poses challenges, as cancer cells can develop resistance to treatments over time.
Genomic instability is a double-edged sword. While it fuels cancer progression, it also creates vulnerabilities that can be therapeutically targeted. By understanding and exploiting these weaknesses, we can develop more effective treatments.
So, as we delve deeper into the hallmarks of cancer, remember: the very chaos that empowers cancer cells might also be their Achilles' heel.
3: "Evading Growth Suppressors: Cutting the Cellular Brakes"
Imagine driving a car downhill with the accelerator stuck and the brakes cut. Terrifying, right? That's essentially what happens in cancer cells when they evade growth suppressors, our third hallmark.
The Role of Tumor Suppressors
In healthy cells, growth is tightly regulated by tumor suppressor genes, which act as the brakes of the cell cycle. Key players include:
p53: Often dubbed the "guardian of the genome," p53 can halt the cell cycle, initiate DNA repair, or trigger apoptosis if damage is irreparable.
RB (Retinoblastoma protein): Regulates the cell's progression from the G1 to S phase, ensuring cells only divide when appropriate.
When these suppressors are inactivated—through mutations, deletions, or epigenetic changes—cells lose critical control mechanisms, leading to unchecked proliferation.
Mechanisms of Evasion
Cancer cells employ various strategies to bypass growth suppression:
Mutations: Alter the structure and function of suppressor proteins.
Epigenetic Silencing: Methylation (the addition of methyl -CH3 groups to the promoter region of a gene, typically leading to reduced gene expression) of promoter regions can silence tumor suppressor genes without altering the DNA sequence.
Disruption of Signaling Pathways: Interfering with pathways that activate suppressor genes.
These alterations remove the safeguards that prevent abnormal cell growth, contributing to tumor development.
Therapeutic Implications
Understanding how cancer cells evade growth suppressors has led to targeted therapies:
CDK Inhibitors (molecules that block the function of cyclin-dependent kinases , a family of enzymes that regulate the cell cycle): Drugs like palbociclib inhibit cyclin-dependent kinases, restoring control over the cell cycle.
Gene Therapy: Efforts to restore function to mutated tumor suppressor genes are ongoing.
These strategies aim to re-establish the cell's natural braking system, curbing uncontrolled growth.
Evading growth suppressors removes critical checks on cell division, propelling cells toward malignancy. By understanding and targeting these mechanisms, we can develop therapies that restore balance and inhibit cancer progression.
So, as we delve deeper into the hallmarks of cancer, remember: restoring the brakes can be just as crucial as cutting the accelerator.
4: The Suicide Squad That Never Showed Up — Resisting Cell Death
Next up on our trip through the twisted theme park of cancer biology — a stop at the haunted house. The exit is clearly marked. The ride is supposed to end. But the monster? He just won’t die.
Let’s talk about apoptosis — aka, the “self-destruct mode” every good, well-mannered cell is born with.
Imagine this: You’re in a Modern Family episode. Phil Dunphy is trying to fix the toaster. Again. But instead of calling an electrician, he wires it to the dishwasher, the lamp, and somehow the neighbor’s WiFi. Eventually, Claire unplugs it and says, “Phil. You’re done.” That’s apoptosis.
It’s the cell’s version of Claire — a quality control system, kicking in when something’s gone haywire: DNA damage, viral invasion, aging, or even when the cell just grows too independent for its own good.
The process is tidy. Controlled. No drama. The cell literally shrinks, chops itself into membrane-wrapped bite-sized vesicles, and gets phagocytosed (eaten) by nearby cells.
But cancer cells? They're the rogue toast-ovens of the universe. They’ve snipped the wires to their own off switch.
How?
Let’s talk mechanisms.
First off: p53. Yes. Our old friend from Episode 1. The boss. The Tony Stark of cell-cycle control. One of his big gigs? Ordering apoptosis when DNA damage gets out of hand. But when p53 is mutated (as it is in over 50% of human cancers), this whole self-destruct protocol becomes optional. And optional is a dangerous setting.
Another important player is Bcl-2 — and no, that’s not a Star Wars droid.
Bcl-2 stands for B-cell lymphoma 2, one of the first discovered anti-apoptotic proteins. Think of it as a bouncer stationed at the mitochondria’s door. Normally, if things go south, mitochondrial outer membranes become permeable, releasing cytochrome c and activating caspases — enzymes that execute apoptosis like efficient ninjas.
But Bcl-2? It bars the door and says, “No ninjas today.”
And it’s not just Bcl-2. There’s a whole family feud between pro-apoptotic (like Bax and Puma — love those names) and anti-apoptotic proteins. The cancer cell tips the balance in favor of the survivalists.
That's not it. There's another villain in the mix: IAPs (inhibitor of apoptosis proteins). These proteins bind to caspases and block their slicing-and-dicing action. Some cancers crank up IAP expression like a Spotify playlist on repeat.
In Stranger Things terms: If apoptosis is the Upside Down claiming messed-up cells, cancer is Vecna, making sure no one gets taken unless he says so.
Now, why does this matter?
Because apoptosis is our first line of defense. It’s why we don’t all turn into blob monsters after sunburns. It’s how your body quietly eliminates ~50–70 billion cells per day. Yes. Per day.
When that mechanism fails?
Mutated cells persist. They divide. They pass on errors. They build resistance to therapy. In fact, many chemotherapy drugs and radiation therapies work by triggering apoptosis in fast-dividing cells. But when cancer cells become resistant to apoptosis, treatment stops working.
Fun (but terrifying) fact: Some cancer cells even secrete survival factors into their microenvironment — little messages to their neighbors like, “Don’t die, buddy. We’ve got this.”
So how do researchers respond? By designing BH3 mimetics (drugs that inhibit Bcl-2), SMAC mimetics (to block IAPs), and more.
Bottom line: Cancer cells refuse to die. They’ve blocked every emergency exit. They’ve unplugged the fire alarms. And they’re partying in a burning building, inviting their mutated friends.
5: Proliferation on Steroids — Sustaining Chronic Proliferative Signaling
Ladies and gentlemen, buckle up — we’re entering the perpetual motion machine part of the cancer circus. Where the ‘on’ button is duct-taped down, and no one remembers where the brakes are.
At the heart of it all — the core behavior that defines cancer — is this: cells that just. won’t. stop. dividing.
Now, a normal cell is like your average high school student. Procrastinates, waits for a signal (“You may now enter S phase”), checks the calendar (a.k.a. checkpoint proteins), and only divides when absolutely necessary — like for growth, repair, or, in high school terms, the night before finals.
But a cancer cell? It’s a Red Bull-fueled maniac running into mitosis like it's Coachella. Again. And again. And again.
Let’s break it down.
The normal cell cycle is governed by signals from growth factors — special proteins (like EGF, PDGF, FGF) that bind to receptors on the cell membrane. These receptors — like the famous EGFR (epidermal growth factor receptor) — are basically antennae that detect the outside world and transmit signals inward.
Once activated, these receptors kick off a cascade of intracellular events — most famously through the RAS–RAF–MEK–ERK pathway. Yes, it sounds like a Hogwarts spell, but it’s essentially a biochemical relay race, ending in the nucleus where genes are turned on to drive cell growth and division.
In many cancers, these receptors are mutated to be constantly active — like a light switch stuck in the “on” position, even when there’s no growth factor around. For example:
HER2 (a relative of EGFR) is amplified in certain breast cancers — too many copies, leading to hypersensitivity and overgrowth.
EGFR mutations are common in non-small cell lung cancers and glioblastomas.
RAS — one of the most frequently mutated oncogenes in human cancer — becomes permanently locked in its “active GTP-bound” form, constantly sending division signals.
So instead of waiting for a growth factor to arrive politely and knock, these cancer cells are like, “I AM the growth factor. I AM the signal.”
Even worse: Some tumors produce autocrine signals — they secrete their own growth factors and then respond to them. Like writing yourself love letters and swooning at them.
Also, mutations in downstream players like PI3K, AKT, or mTOR allow for even more runaway signaling. These molecules control not just growth but metabolism, survival, and protein synthesis. It’s a triple threat — and the cancer cell has VIP backstage access.
Let’s not forget MYC — a powerful transcription factor (on chromosome 8) often overexpressed in cancers like Burkitt lymphoma. It turns on genes involved in metabolism, ribosome biogenesis, and more — basically the cell’s fuel station. An overactive MYC says, “More ribosomes! More mitochondria! More everything!” And cancer says, “Yes, chef.”
And what about the normal brakes on proliferation? Growth suppressors like Rb (retinoblastoma protein) are often inactivated in cancer.
Why does this matter? Because unchecked proliferation leads to tumor growth. A single mutant cell divides into two… then four… then eight… and soon you have a mass of a billion cells (roughly the size of a pea). And it doesn't stop there.
You know that one kid in school who wouldn’t stop talking, even when the teacher glared? That’s a cancer cell on proliferative steroids. Only instead of detention, it gets immortality.
6: Fueling the Fire — Altered Metabolism
“You are what you eat.”🧬 Unless you’re a cancer cell, in which case... you eat like a maniac at a Vegas buffet, 24/7, carbs first.
Welcome to the gluttonous underworld of cancer cell metabolism—aka the “Warburg Wonderland.”
In normal human cells, energy is generated primarily through a process called oxidative phosphorylation in the mitochondria. It’s like your Tesla plugging in to a power station—clean, efficient, and dependent on oxygen. But cancer cells? Oh no, they’re stuck in a Fast & Furious loop of metabolic chaos.
Back in the 1920s, scientist Otto Warburg noticed something odd: even when oxygen is abundant, cancer cells prefer aerobic glycolysis—breaking down glucose into lactic acid. Think of it like choosing to charge your Tesla with a hamster wheel instead of an EV charger. Makes zero sense… until it does.
Why? Because aerobic glycolysis, though inefficient for producing ATP (energy), offers cancer cells two major perks:
Speed – It’s way faster than oxidative phosphorylation.
Building Blocks – It provides intermediates for biosynthesis (lipids, nucleotides, amino acids). Cancer cells aren’t just powering themselves—they’re building empires.
It’s like they’re not just burning calories, they’re using the leftover ash to build secret lairs. Sneaky.
This metabolic reprogramming is often driven by oncogenes like MYC and RAS, which hijack glucose transporters (GLUT1), enhance glycolytic enzymes, and even tweak the TCA cycle. Meanwhile, p53, our fallen hero, typically helps regulate mitochondrial respiration. But when he's MIA, glycolysis parties on.
This is basically Rachel and Chandler in the episode “The One With the Cheesecake”—they know they shouldn’t, but they dive face-first into a cheesecake fallen on the hallway floor. Repeatedly. Cancer cells and glucose? Same energy.
And it’s not just glucose. Some tumors become glutamine addicts, relying on this amino acid to support rapid division. Others exploit the pentose phosphate pathway to make nucleotides and antioxidants. These adaptations allow cancer cells to resist oxidative stress, another weapon the body tries to use to stop them.
This altered metabolism is so consistent across cancers that researchers are developing drugs to target these pathways. But keep in mind—this metabolic shift isn’t just for survival. It’s for domination.
So, next time someone says “Cancer feeds on sugar,” they’re... kind of right. But it’s not just about snacks. It’s a full-blown, rewired metabolic strategy—a buffet designed to serve chaos.
Segment 7: Master of Disguise — Avoiding Immune Destruction
“You can’t fight what you can’t see.” Especially if it looks exactly like you.
The immune system is Earth’s OG Secret Service. It scans, detects, and eliminates suspicious activity like a pro. But cancer? It’s the Tom Riddle of biology—charming, deceptive, and always one step ahead.
Normally, immune cells like T lymphocytes, natural killer (NK) cells, and macrophages are constantly surveilling the body, hunting for rogue cells. They’re the Hogwarts professors keeping an eye out for dark magic. But cancer cells learn how to slip through the cracks—wearing invisibility cloaks, changing their passwords, and sometimes, inviting the guards to tea.
Let’s break down a few of their favorite tricks:
1. Downregulating MHC molecules
MHC I molecules present proteins from within the cell to the immune system. When cells go rogue, they typically display abnormal proteins via MHC I. Cytotoxic T cells see this and go full Avada Kedavra.
Cancer cells, however, often reduce MHC I expression to hide their mutations. It’s like Photoshopping your mugshot out of the “Wanted” poster.
2. Upregulating immune checkpoint proteins
This is the real-life equivalent of saying, “Hey, I’m one of you,” and showing a fake badge. Tumor cells often overexpress proteins like PD-L1, which bind to PD-1 receptors on T cells and turn them off.
It’s the Michael Scott approach to conflict: “I declare bankruptcy!” and hope the problem disappears.
Immune checkpoint inhibitors—like anti-PD-1 or anti-CTLA-4 drugs—aim to lift this suppression and reawaken immune attacks. That’s the idea behind revolutionary immunotherapies.
3. Recruiting Tregs and M2 Macrophages
Tumors don’t just hide—they manipulate. They recruit regulatory T cells (Tregs) that suppress immune responses and M2-polarized macrophages that promote tissue repair, not destruction.
4. Shedding stress ligands
Some tumors remove activating ligands from their surface that NK cells look for. Like when Dwight Schrute disables the office fire alarms so he can fake a fire drill.
This hallmark is especially important in cancers like melanoma and lung cancer, where immune checkpoint therapy has made major strides.
So why doesn’t the immune system always win?
Partly because of this elaborate camouflage, and partly because of immunoediting—the evolutionary process where highly visible cancer cells are destroyed early, and the stealthiest, most deceptive ones survive.
It’s natural selection at its darkest: survival of the slipperiest.
8: Fire That Fuels — Tumor-Promoting Inflammation
🎤 “Inflammation: the body’s version of a fire alarm.”🧬 But what happens when the fire alarm won’t shut up… and the fire actually starts enjoying it?
Let’s get one thing straight: inflammation is not the enemy. It’s your body’s first responder. Whether it’s a stubbed toe or a flu virus, inflammation rushes in with sirens blaring—swelling, redness, heat, and pain—all in a bid to clean house and promote healing.
But in cancer, inflammation goes rogue. It’s no longer the firefighter—it’s the pyromaniac.
Chronic inflammation is like that one guy at a party who was fun for the first hour but is now punching holes in your drywall and refusing to leave. Over time, it becomes a toxic environment that fuels the very thing it was supposed to stop.
Inflammatory Cells: Friends Turned Frenemies
Cells like macrophages, neutrophils, and T-cells infiltrate tumor sites and release a storm of cytokines—TNF-α, IL-6, IL-1β—all of which, ironically, promote tumor growth.
How? By:
Inducing DNA damage (cue genome instability),
Promoting angiogenesis (hello, blood supply),
Inhibiting apoptosis (no death? No problem),
And creating an immunosuppressive environment (as in: “cancer, you do you”).
In fact, some tumors are literally addicted to inflammatory signals. It’s like giving the Joker unlimited access to Gotham’s power grid.
Examples?
Hepatitis B/C viruses cause liver inflammation → increased risk of hepatocellular carcinoma.
Helicobacter pylori causes chronic gastric inflammation → gastric cancer.
Ulcerative colitis and Crohn’s disease → higher risk of colorectal cancer.
Molecular Mischief
Inflammation activates transcription factors like NF-κB and STAT3, which regulate genes involved in proliferation, survival, angiogenesis, and invasion. Cancer hijacks these pathways like a hacker breaking into your Netflix account and replacing your watchlist with 200 hours of "How to Take Over the World."
Stranger Things fans? Think of inflammation like Vecna’s curse—it starts slow, subtle, and insidious. By the time you realize something’s wrong, you’re levitating off the floor and your eyeballs are doing gymnastics.
Therapeutic Insight:
Anti-inflammatory drugs like NSAIDs and corticosteroids are being studied as potential adjuncts in cancer therapy. The goal? Stop fanning the flames before they become a wildfire.
Because here’s the kicker: inflammation doesn't just help tumors start—it helps them thrive.
9: Building Bridges — Induction of Angiogenesis
“What do tumors want?” Same thing as real estate developers: Location. Resources. And, most of all… plumbing.
Imagine building a mansion in the middle of the desert. It’s gorgeous, sinister, full of evil plans… but it has no water. Without blood vessels, even the nastiest tumor is just a sad, shriveled clump of cells.
That’s where angiogenesis comes in: the formation of new blood vessels from pre-existing ones. Normally, it’s a tightly regulated process—essential during wound healing or menstruation. But tumors? They break into the control room and start pushing buttons like toddlers on espresso.
Why Do Tumors Need Blood Vessels?
Because they’re greedy. Blood brings:
Oxygen and glucose (hello altered metabolism!),
Avenue for growth (sustained proliferation),
Escape routes (future metastasis, anyone?),
Growth factors and nutrients galore.
No vessels = no nutrients = no cancer party. So they make sure the party never ends.
Key Molecular Players:
VEGF (Vascular Endothelial Growth Factor): The Beyoncé of pro-angiogenic factors. It binds to VEGF receptors on endothelial cells and says: “Build, baby, build.”
FGF (Fibroblast Growth Factor): Another stimulator of endothelial proliferation.
Angiopoietins, PDGF, and TGF-β also get in on the action.
Tumors secrete these factors in spades, especially under hypoxic conditions. Lack of oxygen triggers HIF-1α, which acts like a biochemical alarm system and unleashes VEGF like a bat signal.
It’s a chemical conga line of construction.
But... Are These Vessels Any Good?
Not really. They’re often:
Leaky,
Disorganized,
Inefficient.
Kind of like trying to irrigate your garden with a straw taped to a firehose. But to the tumor, it’s good enough.
Therapeutic Spotlight:
Enter anti-angiogenic drugs like bevacizumab (Avastin). These drugs aim to starve tumors by blocking VEGF pathways. Results have been mixed—sometimes tumors adapt, sometimes vessels grow back. But it’s a promising strategy.
What’s the takeaway?
Inducing angiogenesis is like building a highway to hell—and then ordering Uber Eats along the way. It’s one of the earliest—and most crucial—steps in a tumor’s long-term survival game.
10: Breaking the Chain — Activation of Invasion and Metastasis
“You thought the tumor staying in one place was bad? Wait till it starts going on road trips.” Metastasis isn’t just an event. It’s an evolution — a villain’s final form.
Let’s be blunt. A tumor that stays put is like a supervillain stuck in traffic. Annoying? Yes. Dangerous? Absolutely. But still manageable.
But once a tumor metastasizes, it goes global. What started as a rogue neighborhood problem in the lungs suddenly becomes a full-blown multi-organ heist.
What Is Metastasis?
It’s the spread of cancer cells from the primary tumor to distant sites. A breast cancer cell might crash the liver. A colon cancer cell might sneak into the brain. Think of it as cancer’s version of Airbnb, only the guests never leave—and trash the place.
It’s not a random escape. It’s a meticulously choreographed sequence, like an Ocean’s Eleven movie… but with a lot more molecular sabotage.
Step-by-Step: The Metastatic Dance
Local Invasion Cancer cells lose their attachments to each other. This is mostly thanks to the downregulation of E-cadherin, a protein that normally acts like emotional glue for cells:“Don’t go! We’re stronger together!”“Nah, I’m off to ruin someone else’s day.”
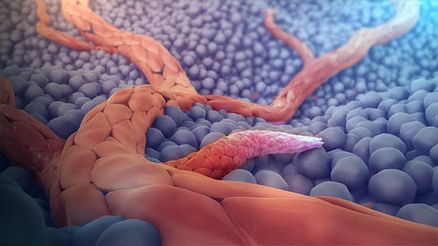
Metastasis of a breast tumor Basement Break-in They penetrate the basement membrane (the tissue layer separating them from the rest of the body) using enzymes like matrix metalloproteinases (MMPs)—molecular bulldozers that smash through structural barriers.
Intravasation Cancer cells slip into the bloodstream or lymphatic system, hitching a ride like microscopic hitchhikers. Not all survive—many get destroyed by shear stress or immune cells.But the smart ones? They cloak themselves using platelets like bio-armor.
Circulation Commute Now they’re in the bloodstream, cruising through arteries and veins like Uber riders of doom. They might only survive a few hours, but some find new organs like kids finding hidden levels in a video game.
Extravasation Time to jump ship. Cancer cells squeeze through blood vessel walls into distant tissues.
Colonization The final—and hardest—step. They need to survive in a foreign land, adapt to its environment, and start dividing again. It’s like moving to a new country, not speaking the language, and still managing to run a billion-dollar empire.
Molecular Players in Metastasis
E-cadherin: Downregulated during metastasis. Its loss is like cutting the safety net.
N-cadherin & Vimentin: Upregulated during epithelial-to-mesenchymal transition (EMT)—a process where epithelial cells become more motile and invasive. Think of EMT like Ross during a normal day (epithelial cell)—awkward, cautious, sweater-loving. Then suddenly, someone eats his sandwich… and boom, he’s yelling “MY SANDWICH?!” and spiraling into chaos (mesenchymal cell).
MMPs: Enzymes that degrade ECM proteins, paving the way for invasion.
Integrins: Help migrating cancer cells latch onto new tissues.
CXCR4/SDF-1 signaling: A GPS system for cancer cells, guiding them toward specific organs.
Why Is Metastasis So Dangerous?
Because metastatic tumors are:
Harder to detect,
Often resistant to therapy,
Spread across multiple systems,
And responsible for ~90% of cancer-related deaths.
Your primary tumor might be manageable. But a second site in the brain, lungs, or liver? That’s a whole new battlefront.
And here’s the kicker: each metastasis is genetically distinct. Like evil clones, they adapt and evolve independently. That’s why personalized therapy is so crucial.
Treatments & Hope
Drugs like metastasis inhibitors are in the pipeline.
Targeting EMT, MMPs, and integrins is showing promise.
Immunotherapies are learning how to sniff out metastatic cells earlier.
But the key lies in early detection and halting the journey before it begins.
Metastasis is Voldemort hiding Horcruxes all over the place. You thought you destroyed the diary? Surprise! There's one in a cup. And a snake. And your brainstem. To truly beat cancer, we need to find every Horcrux, no matter how well it’s hidden.
“Cancer isn’t just a disease of growth. It’s a disease of rebellion. Of cells saying, ‘Forget the rules—we’re going global.’”
And that’s why understanding metastasis isn’t just academic—it’s existential. Because if we stop this one hallmark, we might just save millions.
So, what have we learned? That cancer isn't just one thing—it’s ten terrifying things. It’s a rebel army that defies growth rules. A shapeshifter that dodges death. A hacker of metabolism. A rogue cell that travels continents in your body like it’s taking a gap year."
"It’s also strangely... poetic. A normal cell, one of your own, just trying to survive. And then—a mutation. One change and suddenly, it forgets who it was. It forgets it was part of a community. It stops whispering ‘live carefully’ and starts screaming ,'Grow. Don’t die. Ignore the rules. Escape. Conquer.'
But we are not powerless.
We are scientists. We are doctors. We are teenagers who obsessed with Stranger Things . We are students just trying to get through tomorrow. We are sisters, brothers, children of uncles who fought hard and smiled harder. We are storytellers with pipettes, warriors with whiteboards, comedians who cry into microscopes and still make jokes like Chandler.
Cancer has ten hallmarks. But so do we. Ten reasons to fight.💪👊 Ten billion cells that still follow the rules. Ten moments a day to laugh, love, live.😊😍😎💩
And if one cell can go rogue and destroy…imagine what one person can do to heal.💞









Comments
Post a Comment